We have finally done our first human trials using the CRISPR gene editing technology. First in China, and now a similar one is likely going to follow in the US.
This was reported on recently by Scientific American and Nature
What Is CRISPR You Ask?
CRISPR is a gene-editing technology, where specific gene sequences are cut out from the DNA and replaced with a new ones.
It stands for "Clustered Regularly Interspaced Short Palindromic Repeat".
Not a very catchy name is it?
The basic principle of CRISPR is that it uses a system already present in the human body that checks and edits the genetic code directly. This is useful for any medical condition where the genes are involved. Which actually turns out to be most of them in one way or another!
For a great introduction to CRISPR technology, be sure to check out this podcast by Radiolab.
They dig into the origins of it, and discuss why biologists, doctors, and virologists are getting so excited by it. It is a revolutionary form of medicine that will likely replace most of our current cancer therapies... if these human trials go as well as planned.
What Will The First Human Trial Involve?
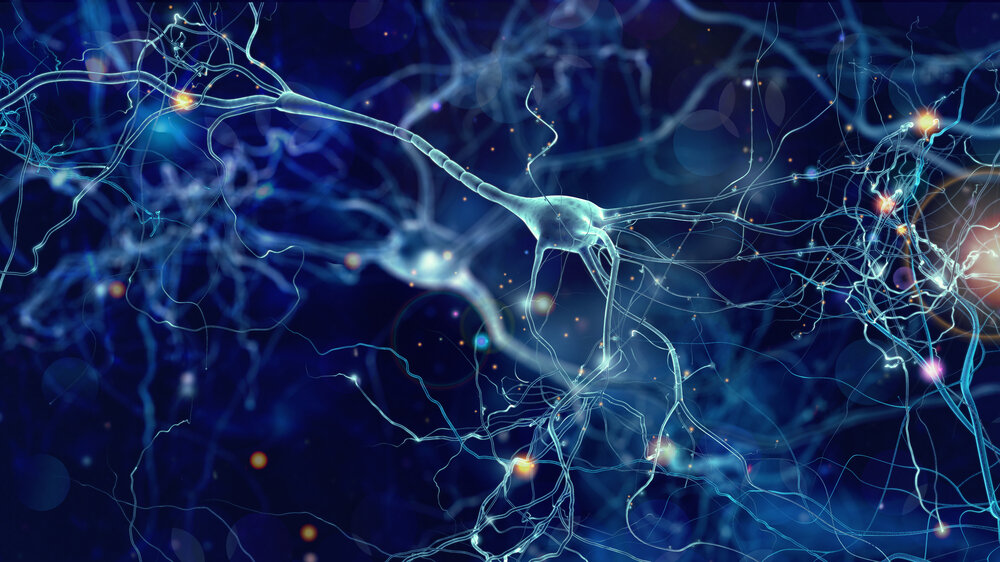
The most recent (and first human) trial in China involved a modification to the gene that encodes a protein known as PD-1.
This protein basically acts to prevent the T-cells (the main soldier cells of the immune system) from attacking healthy cells. Issues with this gene is one of the causes for autoimmune diseases. Cancer cells can exploit this gene to hide themselves from the attacking T-cells.
This allows them to remain undercover while they grow and spread throughout the body.
There is a drug currently used in cancer treatment that works by inactivating this protein, but it's unreliable as to how far the drug can go.
This is because with drug therapies, the drug needs to physically bump into the target cell to work. An impossible feat when you consider how much surface area the blood vessels have in the human body.
If stretched end to end, all of the blood vessels would stretch 160 000 kms (100 000 miles). That amount distance makes drug therapies challenging when trying to inactivate proteins on a cell surface.
CRISPR on the other hand has an advantage...
By physically editing this protein out, the effects will be much stronger, affect more T-cells, and will be a lot more reliable.
After removing this protein, scientists believe the modified T-cells will have a much greater success with attacking the lung cancer cells in the terminally ill patients.
How was it done?
There are several steps. First the patients T-cells are extracted, before CRISPR-Cas9 technology is used to remove the coding sequence for the PD-1 protein. These T-cells will then be checked by collaborator and biotechnology company Chengdu MedGenCell for any misguided edits.
The approved cells will then be cultured and multiplied before being injected back into the patient. In essence, a few are treated and edited with CRISPR, then once found to have been successful, these cells are reproduced into the millions in petri dishes and test tubes and injected back into the body.
This process will greatly improve the down regulation of this PD-1 protein, which is believed to hinder the ability for these T-cells to recognize and fight the cancer effectively.
Using Supportive Agents
There are several supportive agents that may greatly improve the success of this treatment. First of all, the patients that will be treated in this human trial were only selected because chemo- and radiation therapy did not work on them.
This is a sort of last resort for these patients. It is well known that after a course of these treatments, T-cell counts become very low. It will be important to raise these numbers beforehand in order to extract an adequate number without having to remove too much blood from the already terminally ill patient.
In current cancer treatment, a slurry of treatments is often used, in an attempt to combat this highly complex disease from multiple angles. Anti-angiogenic to prevent the tumors from supplying itself with new blood and waste channels, apoptotics to improve the programmed cell death of cancerous cells, and immunostimulants to improve the bodies natural ability to kill the cancerous cells.
The current CRISPR trial will take on an approach of using the bodies own immune system to target and kill the cancerous cells. Supplementing this, with other anticancer mechanisms may have a much higher success rate when used in conjunction.
Substances such as cannabis, with well known anticancer benefits by providing apoptosis modulating, and anti-angiogenic attributes, as well as reishi, turkey tail fungus, and chaga, may all play synergistic roles in the treatment of cancer using CRISPR in this particular application.
Autoimmunity
When you cut out the defence mechanism for preventing a T-cell from attacking the bodies own cells, it will no doubt begin to attack the bodies own cells.
This is a major problem for obvious reasons. Supportive therapies will likely involve treating the side effects of this process and repairing the damage after the fact with nutritional and vitamin supplementation, and antioxidant therapies.
Final notes
The current trial plans will not use any of these, and there are likely to be unforeseen complications with this newly developed method.
It’s important to consider ways to improve, and test supplemental therapies when the time is right.
There's always room for improvement, especially in the world of medicine.
As we adapt and develop new ways of treating disease, we need to learn how to incorporate this into our medical system as effectively and safely as we can and use what we already have and understand to our advantage.