What is Lion's Mane?
Lion's mane is a medicinal wood-rotting fungus with a characteristic growth pattern that resembles the shaggy mane of a lion.
The fungus prefers temperate forests in North America, Europe, and Asia where it thrives on living oak, beech, or conifer trees.
The medicinal benefit of lions mane primarily involve the nervous system. Modern applications use the mushroom for general cognitive health and as a natural nootropic substance.
This mushroom is also eaten as a delicacy — with a flavor similar to lobster when cooked with butter.
In recent years lion's mane has caught the eye of the nootropic community for its ability to up-regulate nerve growth factor.
Top Lion’s Mane Products
Host Defense Lion’s Mane Capsules
Host Defense Lion’s Mane Tincture
Host Defense Stamets 7
How Is Lion's Mane Used?
Lion's mane is mainly used for neurodegenerative disorders like dementia and multiple sclerosis. It's also popular as a nootropic agent for supporting optimal cognitive function long term.
Most of the people using this fungus take it in the form of a powdered capsule or tincture on a daily basis. Like most medicinal mushrooms, the biggest benefit comes from using the herb on a regular basis over long periods of time — rather than short bursts for quick impact of effects.
Traditional Use of Lion’s Mane
Lion’s mane mushrooms have a long history of use in Eastern Asia — including China, Korea, and Japan. Each of these regions used the mushroom for treating neurological disorders, including neurasthenia, and age-related cognitive decline, as well as for general health.
Herb Details: Lion's Mane
Herbal Actions:
- Antibacterial
- Anticancer
- Antidiabetic
- Antioxidant
- Cardioprotective
- Hepatoprotective
- Nervine
- Immunomodulator
Weekly Dose
- (1:2 Liquid Extract)
20-60 mL - View Dosage Chart
Part Used
- Fruiting Body
Family Name
- Hericiaceae
Distribution
- North America, Europe, Russia, Mountainous regions of Asia
Constituents of Interest
- Hericnones
- Erinacines
- Lactones
- Polysaccharides
Common Names
- Lion's Mane
- Monkey's Head
- Hedgehog Fungus
- Pom Pom
- Houtou (China)
- Shishigashira (China)
- Yamabushitake (Japan)
Pregnancy
- Safe during pregnancy.
Duration of Use
- Long term use acceptable and recommended.
Mycological Information
The Hericiaceae family of fungi are saprophytic (consumes dead wood), yet can be found growing on living trees as well. Many experts believe the mushroom has a mutualistic relationship with the tree for some time — helping it resist disease and infection, but will eventually consume the tree after it dies.
Hericium mushrooms normally grow in cooler, mountainous regions across the globe. It contains a number of species used medicinally and nutritionally.
Hericium spp. has characteristic "tooth" structures on its fruiting body, giving it a hair-like appearance.
Pharmacology & Medical Research
+ Neuroprotective
Lion’s mane offers several different mechanisms to produce its overall neuroprotective benefits:
- Antioxidant and free-radical scavenging activity [6]
- Anti-inflammatory activity
- Nerve-growth factor stimulation (hericium and erinacenes)
- Reduction of endoplasmic reticulum stress-dependant cell death (dilinoleolyl-phosphatidylethanolamine (DLPE) [7]
- Attenuation of beta-amyloid-related cognitive decline in animals (dementia model) [8]
- Enhance mylenation of neurons [9, 10, 11]
In animal studies, lion’s mane has been shown to reduce the severity of damage after a stroke — effectively protecting the sensitive neurons from ischemic damage [6].
Clinical Trials:
Study: Mori et al., 2009 — Improving effects of the mushroom Yamabushitake (Hericium erinaceus) on mild cognitive impairment: a double‐blind placebo‐controlled clinical trial. [5]
This randomized, double-blind, placebo-controlled clinical trial involving 30 Japanese men and women with mil cognitive impairment found that after 16 weeks, the lion’s mane group had significantly increased cognitive scores. These improvements were noted as early as the 8 week checkup, and continued to improve compared to placebo over the rest of the 16-week trial.
The dose of lion’s mane used in this study was 1 gram of dried lion’s mane taken three times per day.
Unfortunately, 4 weeks after the trial concluded, the scores had significantly decreased — indicating that these effects are not permanent and the mushroom needs to be continued to remain effective.
+ Nootropic
A nootropic is a substance that improves cognition without causing harm. There are a lot of nootropic substances that range from herbs like lion’s mane or rhodiola, to synthetic or prescription drugs like Modafinil or Noopept.
Lion’s mane is thought to be a nootropic through its ability to promote nerve-growth factor (NGF) in the brain. NGF is the most potent growth factor for the cholinergic neurons. it influences everything from the proliferation, differentiation, and survival of neuronal cells in the brain [8, 12].
Reductions in NGF has been considered a major implication in conditions such as depression, substance abuse, Alzheimer’s disease, and Huntington’s disease [12].
There have been a lot of studies looking at the role of lion’s mane and nerve growth factor — most of which have concluded that lion’s mane applications directly lead to an increase in NGF. This research has been done both in vivo and in vitro [13, 14, 15, 16].
This effect is very important. We can give peptides like NGF to people to treat these neurodegeneration, but these peptides rarely cross the blood brain barrier [9]. Therefore, finding alternative ways to boost NGF or other peptides in the brain are of the utmost importance in the treatment, prevention, and management of neurodegenerative disorders.
+ Immunomodulation
Like many other medicinal mushrooms, lion’s mane contains a high concentration of polysaccharides with immunomodulatory effects.
A lot of this study has been done in vitro with dendritic immune cells. These cells serve as the antigen-presenting cells that act as central mediators for the immune response as a whole. They’re responsible for a lot of the tolerance formed by the immune system to help maintain homeostasis.
Studies involving lions mane extracts have shown the fungus can stimulate the maturation of dendritic cells, induce dendritic cell activation, and modulate key T-helper (Th1) immune responses [17].
+ Anti-Inflammatory
Lion’s mane has been shown to influence a variety of inflammatory mediators, including:
Induces IL-1β expression through Nf-kB, NF-IL6, and activator protein 1 (AP-1) [18]
Induces iNOS gene expression to increase nitric oxide (NO) production in macrophages
Inhibits toll-like receptor 4 (TLR4)-JNK signalling on macrophages [19]
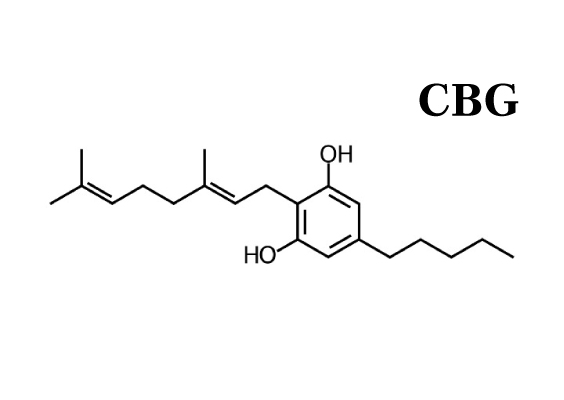
Phytochemistry of Lion’s Mane Mushrooms
Lion’s mane fruiting body and myclelia contain an exceptionally diverse range of unique bioactive substances — including polysaccharides, meroterpenoids (hericinones), cyathane diterpenoids (erinacines), steroids, alkaloids, and lactones.
The most significant constituents in terms of the mushrooms medicinal action are the hericenones and erinacines. Both of these substances have been shown to stimulate nerve growth factor in the central nervous system. This is thought to be the primary mechanism for which the fungus an improve the health and function of the nervous system.
Clinical Applications Of Lion's Mane:
Lion's mane has many uses, but the most well-known is as a neuroprotective, and nootropic benefits. It's useful for neurodegenerative disorders including multipple sclerosis, Alzheimer's disease, and Parkinson's disease.
Other uses include depression and anxiety, cancer, diabetes, gastrointestinal infection, and fatigue.
Cautions & Safety
Lion’s mane is a culinary mushroom that’s been used for both food and medicine by countless individuals over several hundreds of years. There are no expected short-term or long-term side effects from using the fungus.
Throughout the clinical research there have been no reports of serious side effects from using the fungus — including very high-potency extracts and long-term durations of use.
Caution advised with any blood clotting conditions or medications due to possible agonistic interactions — including haemophilia or other bleeding disorder, thrombocytopenia, or post-surgery. Lion’s mane may interact with blood thinners or anti-platelet medications.
Recent Blog Posts:
References
[1] — Friedman, M. (2015). Chemistry, nutrition, and health-promoting properties of Hericium erinaceus (lion’s mane) mushroom fruiting bodies and mycelia and their bioactive compounds. Journal of agricultural and food chemistry, 63(32), 7108-7123.
[2] — Liu, J., Du, C., Wang, Y., & Yu, Z. (2015). Anti-fatigue activities of polysaccharides extracted from Hericium erinaceus. Experimental and therapeutic medicine, 9(2), 483-487.
[3] — Thongbai, B., Rapior, S., Hyde, K. D., Wittstein, K., & Stadler, M. (2015). Hericium erinaceus, an amazing medicinal mushroom. Mycological progress, 14(10), 91.
[4] — Wong, K. H., Naidu, M., David, R. P., Bakar, R., & Sabaratnam, V. (2012). Neuroregenerative potential of lion's mane mushroom, Hericium erinaceus (Bull.: Fr.) Pers.(higher Basidiomycetes), in the treatment of peripheral nerve injury. International journal of medicinal mushrooms, 14(5).
[5] — Mori, K., Inatomi, S., Ouchi, K., Azumi, Y., & Tuchida, T. (2009). Improving effects of the mushroom Yamabushitake (Hericium erinaceus) on mild cognitive impairment: a double‐blind placebo‐controlled clinical trial. Phytotherapy Research, 23(3), 367-372.
[6] — Lee, K. F., Chen, J. H., Teng, C. C., Shen, C. H., Hsieh, M. C., Lu, C. C., ... & Huang, W. S. (2014). Protective effects of Hericium erinaceus mycelium and its isolated erinacine A against ischemia-injury-induced neuronal cell death via the inhibition of iNOS/p38 MAPK and nitrotyrosine. International journal of molecular sciences, 15(9), 15073-15089.
[7] — Nagai, K., Chiba, A., Nishino, T., Kubota, T., & Kawagishi, H. (2006). Dilinoleoyl-phosphatidylethanolamine from Hericium erinaceum protects against ER stress-dependent Neuro2a cell death via protein kinase C pathway. The Journal of nutritional biochemistry, 17(8), 525-530.
[8] — Mori, K., Obara, Y., Moriya, T., Inatomi, S., & Nakahata, N. (2011). Effects of Hericium erinaceus on amyloid β (25-35) peptide-induced learning and memory deficits in mice. Biomedical Research, 32(1), 67-72.
[9] — Phan, C. W., David, P., Naidu, M., Wong, K. H., & Sabaratnam, V. (2015). Therapeutic potential of culinary-medicinal mushrooms for the management of neurodegenerative diseases: diversity, metabolite, and mechanism. Critical Reviews in Biotechnology, 35(3), 355-368.
[10] — Kolotushkina, E. V., Moldavan, M. G., Voronin, K. Y., & Skibo, G. G. (2003). The influence of Hericium erinaceus extract on myelination process in vitro. Fiziol Zh, 49(1), 38-45.
[11] — Moldavan, M., Grygansky, A. P., Kolotushkina, O. V., Kirchhoff, B., Skibo, G. G., & Pedarzani, P. (2007). Neurotropic and trophic action of lion's mane mushroom Hericium erinaceus (Bull.: Fr.) Pers.(Aphyllophoromycetideae) extracts on nerve cells in vitro. International Journal of Medicinal Mushrooms, 9(1).
[12] — Chao, M. V., Rajagopal, R., & Lee, F. S. (2006). Neurotrophin signalling in health and disease. Clinical science, 110(2), 167-173.
[13] — Zhang, C. C., Yin, X., Cao, C. Y., Wei, J., Zhang, Q., & Gao, J. M. (2015). Chemical constituents from Hericium erinaceus and their ability to stimulate NGF-mediated neurite outgrowth on PC12 cells. Bioorganic & medicinal chemistry letters, 25(22), 5078-5082.
[14] — Samberkar, S., Gandhi, S., Naidu, M., Wong, K. H., Raman, J., & Sabaratnam, V. (2015). Lion's Mane, Hericium erinaceus and Tiger Milk, Lignosus rhinocerotis (Higher Basidiomycetes) medicinal mushrooms stimulate neurite outgrowth in dissociated cells of brain, spinal cord, and retina: an in vitro study. International journal of medicinal mushrooms, 17(11).
[15] — Lai, P. L., Naidu, M., Sabaratnam, V., Wong, K. H., David, R. P., Kuppusamy, U. R., ... & Malek, S. N. A. (2013). Neurotrophic properties of the Lion's mane medicinal mushroom, Hericium erinaceus (Higher Basidiomycetes) from Malaysia. International Journal of Medicinal Mushrooms, 15(6).
[16] — Mori, K., Obara, Y., Hirota, M., Azumi, Y., Kinugasa, S., Inatomi, S., & Nakahata, N. (2008). Nerve growth factor-inducing activity of Hericium erinaceus in 1321N1 human astrocytoma cells. Biological and Pharmaceutical Bulletin, 31(9), 1727-1732.
[17] — Sheu, S. C., Lyu, Y., Lee, M. S., & Cheng, J. H. (2013). Immunomodulatory effects of polysaccharides isolated from Hericium erinaceus on dendritic cells. Process biochemistry, 48(9), 1402-1408.
[18] — Son, C. G., Shin, J. W., Cho, J. H., Cho, C. K., Yun, C. H., & Han, S. (2006). Induction of murine interleukin‐1 beta expression by water‐soluble components from Hericium erinaceum 1. Acta Pharmacologica Sinica, 27(8), 1058-1064.
[19] — Mori, K., Ouchi, K., & Hirasawa, N. (2015). The anti-inflammatory effects of lion's mane culinary-medicinal mushroom, hericium erinaceus (higher basidiomycetes) in a coculture system of 3t3-L1 adipocytes and raw264 macrophages. International journal of medicinal mushrooms, 17(7).






































As COVID-19 continues to spread around the world, we’re getting a lot of questions on what the potential role of herbal medicine is during the outbreak. Learn how the virus works and how to limit your chances of transmission.